Breast Reconstruction after mastectomy
Opting for reconstruction can minimise the psychological impact associated with losing a breast, especially if performed immediately after mastectomy. One study, which compared patients who had undergone breast reconstruction with those who had a mastectomy without reconstruction, found they were significantly more satisfied with their appearance and fared better psychosocially and sexually. Furthermore, they functioned better physically, experiencing less pain and fewer limitations.
Reconstruction without implants
In some cases it is possible to reconstruct a breast exclusively with a patient’s own tissue. Known as “autologous flap” surgery, it involves taking a section of skin, fat and sometimes muscle, from elsewhere on the body and transplanting it to the breast.
So-called “flaps” can be taken from the tummy, buttocks, upper back, inner thigh or upper hip. They can be cut completely free or left partially attached to the blood supply (pedicled) and moved up to the chest from within the body. With “free flap” reconstruction, the blood supply is re-established using microvascular surgery techniques.
The most popular autologous flap method uses the tummy as a donor site. This method has the unintentional benefit of providing patients with a tummy tuck at the same time, due to the relocation of abdominal tissue and subsequent skin tightening.
It can be performed either as free or pedicled, but free flap (DIEP flap) is preferred because it means the rectus abdominis muscle can be spared, helping to preserve abdominal strength.
The reconstructed breast can be further filled and shaped through fat transfer, which involves removing fat from another part of the body via micro liposuction and reinjecting it. Like the transplanted abdominal tissue, the fat regains a blood supply and becomes permanent.
Providing a patient has enough donor fat and tissue on their body, autologous flap surgery can offer an all-natural way to restore the shape and size of their breast. The tissue ages naturally and changes volume corresponding to the patient’s overall body weight. While the patient will be left with scars on the donor site, when the flap is taken from the abdomen, these scars are well concealed below the bikini line.
Reconstruction with implants
If a skin-sparing mastectomy or lumpectomy is performed, where much of the breast skin is preserved, an implant can be immediately implanted under the pectoralis muscle. If the mastectomy leaves the skin too tight, a two-stage implant process is necessary.
Firstly, a tissue expander (essentially a silicone pouch) will be put in and slightly expanded with saline solution. Over a period of several weeks, the expander is expanded via the injection of additional saline solution. This gradually stretches the skin and creates a pocket for the implant.
A new type of expander called AeroForm uses carbon dioxide instead of saline solution. It is needle-free and is expanded by the patient, at home, using a wireless, handheld dosage controller.
When the breast tissue expands to the desired size, the expander is replaced with a permanent implant. The benefit of using implants over autologous flap is that scarring is restricted to the breast itself and the procedure does not rely on the patient having sufficient donor tissue. It is therefore the best option for thinner individuals.
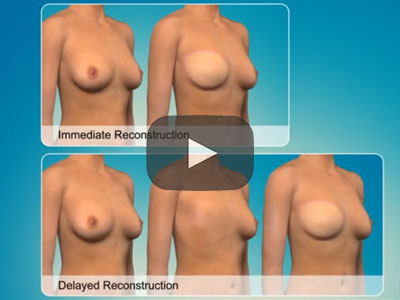
Timing for a breast reconstruction
The best outcomes can be achieved when breast reconstruction is carried at the same time as mastectomy or lumpectomy. Not only does it reduce the number of times a patient must undergo surgery and minimise scarring, deciding on immediate reconstructions enables patients to opt for a skin-sparing surgery.
Most women are eligible for skin-sparing mastectomies (unless the tumour cells are close to the skin). During skin-sparing mastectomy, the surgeon removes only the skin of the nipple, areola, and the original biopsy scar. Then the surgeon removes the breast tissue through the small opening that is created. The remaining pouch of skin provides the best shape and form to accommodate an implant or autologous flap. It enables patients to get the most realistic and pleasing results from breast reconstruction.
If a patient does not opt for immediate reconstruction, a skin-sparing mastectomy is not usually performed. The surgeon will most likely remove as much skin as is required to make the scar and the surface of the chest flat.
If a patient decides to wait and have reconstructive surgery later, they may still choose between an implant or autologous flap. The incision will be made along the scar of the previous mastectomy. In the case of implants, an expander will be used first, which does require the patient to have two operations.
Breast reconstruction and radiotherapy
Radiotherapy can reduce the likelihood of a successful breast reconstruction. This is because radiation kills normal tissue as well as cancerous tissue. It is therefore recommended to delay reconstruction until after treatment has been completed.
Radiated skin is hard to stretch and often becomes discolured. In addition, because radiation therapy significantly increases the risk of capsular contracture (the formation of excessive scar tissue around an implant) delayed autologous flap reconstruction is recommended over reconstruction with implants.
The good news is that, whatever a patient’s treatment plan, reconstruction is almost always an option. And although immediate reconstruction is preferable from a surgical point of view, breast reconstruction can be carried out months or even years after surgery. This means patients can take as much time as they need to recover, whether that’s physically or mentally.
Achieving the best aesthetic result possible
Achieving symmetry between a patient’s breasts is a key goal. To this end, a reconstruction can be carried out in combination with surgery on the remaining breast to ensure they are as close in size and shape as possible.
If the mastectomy has included the removal of the nipple, this can be reconstructed three to four months after surgery. This can be done by creating small flaps at the site where the nipple would have been and forming them into a nipple mound.
Micropigmentation tattoo is then used to simulate the natural colours. Alternatively, micropigmentation alone can used, with colour skillfully applied to give the appearance of a three-dimensional nipple.
While your new breast will never look or feel 100% like your old breast, breast reconstruction surgery can help you feel like your “old self” again, making you more confident to be intimate, on the beach or in the changing rooms.
Ocean Clinic Marbella and Madrid specialises in breast surgery, including reconstruction, reduction, and enhancement. If you are facing the prospect of mastectomy or have already undergone breast removal and would like to discuss your options for reconstruction contact Ocean Clinic in Marbella and Madrid.