Lifting the lid on under-eye fillers: The G Point lift
Under eye fillers are a popular way to restore a youthful look to the face by replacing lost volume to the ‘hollows’ under the eyes. This deformity can be genetic or a part of the ageing process of the cheeks as well as the peri-ocular (under eye) area. When collagen production slows down, fat is lost, bone is reabsorbed, and hollows begin to form under the eyes giving the face a tired and droopy appearance. It can often appear that we have dark circles and a withdrawn look to the eyes and cheeks. Due to the constant advances in aesthetics we are gaining more and more understanding as to why this occurs, the detailed anatomical reasons behind ageing, as well as how best to counter these facial reactions using cosmetic treatments.
A study, led by our very own Gabriela Casabona MD et al. from Ocean Clinic, Marbella, based on where to best position facial soft-tissue fillers, was carried out to look into a new injection protocol which makes use of the advances in the understanding of facial anatomy. The aim was to investigate where best to position injectable soft-tissue fillers considering the line of ligaments (an imaginary line connecting different retaining ligaments and dividing the face into lateral and medial sections) and surface of the face for most efficient volumisation.
Better understanding of the facial anatomy and the layered arrangement of facial soft tissues has introduced a more 3-dimensional approach to minimally invasive treatments, such as soft-tissue fillers. This more extensive knowledge provides information on which layers of the face are more effective or present a greater risk for vascular events. Practitioners are now able to determine more precisely, guided by this information, how the facial fat compartments and boundaries need to be respected, achieving greater aesthetic results and safer outcomes.
This study describes the results of a new injection algorithm respecting newly conceived anatomical concepts. Data received from 306 patients having received the same soft-tissue fillers using the same technique were used to determine the results.
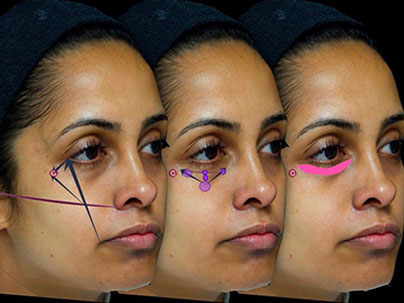
Figure 1: The injection scheme. The face on the far left shows how the G point is determined - a line from the nose to the ear, another from the corner of the mouth to the corner of the eye, and a third from an intersection of the two. The middle face shows where the injection points are allocated and the third depicts the contours.
All patients were treated with the same injection technique, the product was applied using markings made on the skin using the protocol in Figure 1 - the G Point - a combination of this starting point alongside the G-prime effect shown in Figure 2.
The technique was carried out as follows:
A dermal access puncture was performed with a 21G needle 1 cm supero-lateral to the midportion of the nasolabial sulcus. A 22G 50 mm blunt-tip cannula (Dermasculpt) was introduced into the superficial nasolabial fat compartment and advanced in the direction of the G-point. After the level of the infraorbital foramen was passed, the cannula was introduced deeper into the supraperiosteal plane. This “first-superficial-then-deep” cannula advancement technique assured that the infraorbital neurovascular structures and the angular vein were crossed superficially. The correct positioning of the tip of the cannula was digitally controlled and assured that it corresponds to the lateral aspect of the sub-orbicularis oculi fat (SOOF)12 and that it is located lateral to the line of ligaments.7,9,10
In the next step contouring, the cannula was retracted (with- out exiting the facial soft tissues) and re-advanced cranially in the mid-pupillary line. Again, a “first-superficial-then-deep” cannula advancement was performed to assure that the infraorbital neurovascular structures were crossed superficially. Three serial bolus injections were applied in the supraperiosteal plane targeting the upper/middle/lower aspects of the medial SOOF.
Next, the cannula was retracted and re-advanced cranially following the “first-superficial-then-deep” approach positioning another supraperiosteal bolus in the palpebromalar groove, inferior to the orbicularis retaining ligament at the level of the lateral canthus and another bolus in the supraperiosteal plane in the tear trough.
Thus, a total of 6 boluses of soft tissue filler of high visco-elastic characteristics were positioned in the supraperiosteal plane utilizing one single dermal access puncture (Figures 1,3).
Then the contour between the cheek and the lower eyelid was addressed. Dermal access was made by a 23G needle (TSK Laboratory) in the dermal location of the G-point. A 25G 38 mm blunt-tip cannula (Dermasculpt) was introduced into the SOOF without establishing bone contact. The cannula was advanced medially, deep to orbicularis oculi muscle and superior to the orbicularis retaining ligament. During retrograde movement, small amounts of soft tissue filler (low visco-elastic characteristics) were injected (Figures 1,4).
So, each patient received the same amount of soft-tissue filler at the same injection sites using the same algorithm and techniques to determine whether this is an improved and more effective method to administer soft-tissue fillers under the eye.
The statistical analysis results (Descriptive and comparative analyses were performed using SPSS Statistics 23 (IBM), and results were considered significant at a probability level of ≤.05.) showed the following:
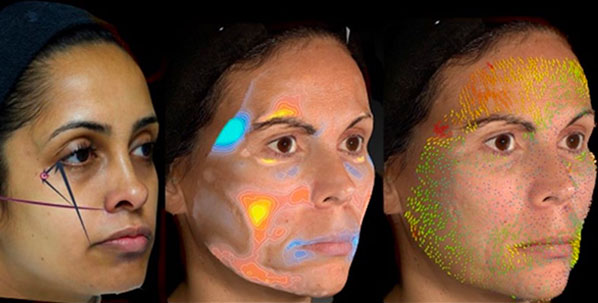
Figure 2: Figure showing the volume changes (middle face) and vectorial skin changes (right face) after injection in the G-point. An increase in volume is represented by dark blue, as a decrease is represented by dark red. Note the laterally oriented skin vectors, indicating a lifting effect after injection into the G-point.
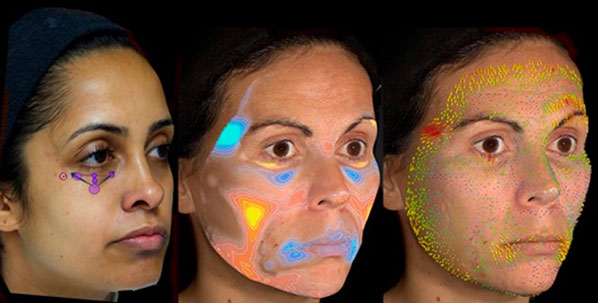
Figure 3: Figure showing the volume changes (middle face) and vectorial skin changes (right face) after injection in the G-point and giving off six infraorbital boluses. An increase in volume is represented by dark blue, as a decrease is represented by dark red.
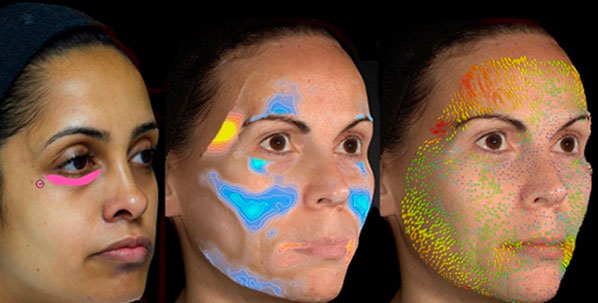
Figure 4: Figure showing the volume changes (middle face) and vectorial skin changes (right face) after injection in the G-point and giving off six infraorbital boluses and infraorbital contouring. An increase in volume is represented by dark blue, as a decrease is represented by dark red.
Conclusion
This clinical study retrospectively analysed a total of 306 patients treated for infraorbital and medial mid-face volume loss according to a standardised injection algorithm. This cannula injection-based algorithm utilises novel anatomic concepts (line of ligaments and surface volume coefficient) and positions the product in the supra-periosteal plane following a “first-superficial-then-deep” cannula advancement technique. The results revealed that utilising these novel anatomic concepts, a mean amount of 0.32 cc high G-prime soft tissue filler injected in the lateral SOOF (G-point) can change mid-facial distances by an average of 0.19 mm. This repositioning of medial mid-facial soft tissues resulted additionally in a reposition of the lower eyelid-cheek junction by an average amount of 0.49 mm.
Put into general terms this means that the result of this study and analysis of this particular style of injection is highly efficient, achieves outstanding results and has an excellent safety outcome. Therefore it seems that the recent anatomical findings and consistent advances in our understanding of every layer and angle of the face has a great impact on the outcome of minimally invasive treatments such as soft-tissue fillers.
